“As sensitivities become more common, the ability to accurately identify and address them becomes essential.”
Understanding food sensitivities is crucial in today’s complex dietary landscape. Many people experience adverse reactions to various foods. Distinguishing between sensitivities, allergies, and intolerances is essential. This distinction helps manage symptoms effectively and improve overall health. Food sensitivities involve delayed immune responses and are increasingly prevalent. Factors include changes in food production and environmental pollutants. Recognizing these sensitivities can significantly impact well-being. In this blog, we explore the causes, identification, and management of food sensitivities for better health.

Understanding Food Sensitivities
In the complex world of dietary health, distinguishing between food sensitivities, allergies, and intolerances is paramount. These terms, often used interchangeably, denote distinctly different phenomena, each requiring a unique approach for identification and management.
Food Allergies represent immediate immune responses. When the body identifies a specific food protein as a threat, it triggers a reaction mediated by Immunoglobulin E (IgE) antibodies. These responses can vary in severity, ranging from mild symptoms to anaphylaxis—a potentially life-threatening condition.
Food Intolerances differ significantly, as they do not involve the immune system. These reactions typically result from the body's inability to digest certain substances, such as lactose in lactose intolerance. They lead to digestive discomfort but do not involve immune-mediated symptoms.
Food Sensitivities are characterized by a delayed immune response, setting them apart from the immediate reactions observed in allergies. These sensitivities involve a slower, more complex process mediated by Immunoglobulin G (IgG) antibodies. The delayed nature of these responses leads to a variety of symptoms, making sensitivities particularly challenging to identify without comprehensive testing.
Navigating the Complexities of Food Sensitivities
The conflation of these terms is more than a semantic issue—it significantly affects individuals' approaches to identification and management. Food sensitivities are increasingly prevalent, a trend attributed to changes in food production and environmental pollutants. Additionally, evolving immune system responses contribute to this rise. Symptoms of food sensitivities can span a wide spectrum, from joint pain and headaches to mood disorders and fatigue. This variety makes it difficult to identify the specific triggers.
Recognizing the fundamental differences between these dietary reactions is crucial in navigating the journey towards optimal dietary health. For food sensitivities, the objective is to pinpoint specific IgG-mediated immune responses. Moreover, these are distinct from the IgE reactions associated with allergies or the digestive issues indicative of intolerances.
This understanding not only aids in managing personal health but also underscores the importance of specialized knowledge for health practitioners. As sensitivities become more common, the ability to accurately identify and address them becomes essential. This highlights the value of continuous learning and expertise in dietary health, inviting professionals to deepen their understanding through specialized certifications.
Identifying Food Sensitivities

Once the distinctions between food sensitivities, allergies, and intolerances are understood, the crucial next step is identifying the specific foods triggering sensitivities. This is essential for managing the often-debilitating symptoms associated with these sensitivities and enhancing overall health and well-being.
The Importance of Testing
Identifying food sensitivities not only improves quality of life by alleviating a wide array of symptoms beyond just gastrointestinal discomfort, such as skin conditions, fatigue, joint pain, headaches, mood disorders, and water retention, but also tailors diets to better support overall health. For individuals with chronic conditions such as inflammatory diseases or autoimmunity, it is crucial to identify and minimize exposure to dietary triggers.
Common Food Sensitivities
A range of foods commonly trigger sensitivities, with the most prevalent including gluten, casein, albumin, soy, and nightshades. These known culprits are useful starting points for individuals beginning to navigate their sensitivities. Identifying these triggers is particularly critical for those with autoimmune conditions due to molecular mimicry. This occurs when the immune system mistakes similar peptides in food for body tissues, exacerbating the condition.
Identifying Trigger Foods
The elimination provocation diet, long regarded as the gold standard for identifying food sensitivities, involves eliminating suspected foods. Afterward, these foods are carefully reintroduced while monitoring symptoms. Developed over decades of clinical practice, this method is highly effective but notably time-consuming and challenging. It is particularly difficult for individuals with busy lifestyles and family responsibilities. In the following section, we'll delve into this and other testing methods, providing a balanced view of available options.
Testing Methods for Food Sensitivities
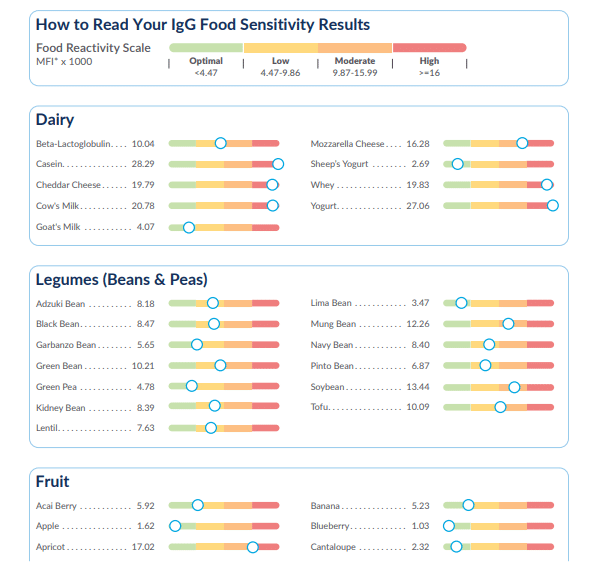
Besides the elimination diet, various testing methods like ELISA (which measures IgG antibodies) offer direct, scientifically validated ways to identify food sensitivities. These methods are particularly useful for those who may find the elimination diet too burdensome. In the next section, we'll dive deeper into these methods, discussing their nuances and how to choose the most reliable one for your needs.
Evaluating Testing Methods
Choosing the right method to test for food sensitivities is as crucial as identifying the sensitivities themselves. The field of food sensitivity testing is diverse, offering various methodologies with distinct advantages and limitations. Here’s a streamlined guide to navigating these options effectively:
Reliable Testing Methods
Among the myriad of testing options, the ELISA (Enzyme-Linked Immunosorbent Assay) test stands out for its precision and reliability. This scientifically validated method measures the immune system's response to specific foods by detecting IgG antibodies, providing a high degree of specificity and sensitivity. Additionally, the accuracy of ELISA is well-supported in immunological literature, making it a trusted choice for both practitioners and patients.
Understanding and Choosing Tests
It’s crucial to differentiate between IgG testing for sensitivities and IgE testing for allergies. Distinguished bodies like the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma, and Immunology emphasize IgG should not be used to diagnose food allergies—for which IgE testing is appropriate—but affirm its utility in assessing food sensitivities.
Navigating Testing Options for Food Sensitivities
While some methods like Cytotoxic testing and certain bioresonance tests claim to evaluate immune responses to foods, they have faced scrutiny and regulatory actions due to inaccuracies and lack of scientific validation. Such tests can lead to false positives and misinterpretations, underscoring the importance of choosing tests like ELISA, which stands as the gold standard in immunology for measuring antibodies related to food sensitivities.
Consulting Healthcare Professionals
When considering food sensitivity testing, it's vital to consult with healthcare professionals who are knowledgeable about the latest methodologies. They can guide you toward the most appropriate tests based on your symptoms and health history, ensuring that the results are interpreted correctly and integrated into a comprehensive dietary management plan.
Addressing Concerns and Misconceptions

In the discussion of food sensitivities, misconceptions can cloud understanding and complicate management. Here, we address common concerns and clarify the facts to empower better health decisions:
Scope of Testing
A prevalent misconception is that food sensitivity testing is unreliable because it only measures immune responses, specifically IgG antibodies. Furthermore, it’s essential to recognize these tests are designed precisely for this purpose—to identify immune reactions to foods, not non-immune reactions such as those caused by maldigestion or food additives. Understanding this scope is crucial for interpreting test results accurately.
Clarifying Literature Confusion
Confusion often arises from a misinterpretation of the literature, where studies incorrectly use IgG (along with IgM and IgA) to evaluate food allergies, not sensitivities. This misinterpretation leads to misleading conclusions about the validity of IgG testing. In truth, immunoglobulin testing is a reliable method for identifying food sensitivities, distinct from allergies, which are more accurately tested with IgE markers.
Reactivity to Cold vs. Cooked Foods
Another point of contention is the belief that food sensitivity testing fails to account for different immune responses to raw versus cooked foods. While cooking can alter a food's antigenicity, this limitation does not negate the utility of testing but highlights the need for a comprehensive dietary analysis. Most ELISA tests focus on reactivity to cold foods; however, understanding how cooking affects reactivity is essential for full dietary management.
Addressing Cross-Reactivity Concerns
Skepticism sometimes arises from instances of cross-reactivity, where tests indicate sensitivities to foods not recently consumed. This occurs because tests target specific amino acid sequences, which can be similar across various foods. Recognizing this complexity helps explain why such results occur, underlining the nuanced nature of immune responses and food sensitivities.
Empowerment Through Understanding
Armed with accurate information and a clear understanding of what food sensitivity tests can and cannot do, individuals and practitioners can navigate the management of food sensitivities more effectively. For those interested in deeper learning or becoming proficient in interpreting these tests for clients, comprehensive training programs can be invaluable. Knowledge empowers us to make informed decisions, leading to more effective management and improved health outcomes.
Beyond Basics: Enhancing Your Health and Professional Skills

As we conclude our exploration of food sensitivities, we've uncovered the importance of a nuanced understanding, accurate identification, and effective management of these complex conditions. Here are our key takeaways and steps forward:
Key Takeaways
- Delayed Immune Response: Understanding the delayed immune response characteristic of food sensitivities is crucial, setting them apart from immediate allergic reactions and highlighting the need for targeted management strategies.
- Reliable Testing: ELISA methodology emerges as a cornerstone for dependable food sensitivity testing, offering a solid basis for pinpointing sensitivities and facilitating dietary adjustments.
- Holistic Management: Effective management of food sensitivities extends beyond mere elimination diets. It encompasses a holistic strategy, considering dietary management alongside underlying health factors, like gut health, for lasting results.
How You Can Make a Difference
- For Practitioners and Aspiring Health Professionals: If you’re navigating the field of health, keen on deepening your grasp of food sensitivities, or aspiring to excel in ELISA test interpretation for your clients, our IHP Level 2 Health Coaching Certification program beckons. Crafted meticulously, this program equips you with comprehensive insights into food sensitivity testing and management. It enables you to confidently and precisely support your clients' health journeys.
- Embrace Continuous Learning: The realm of food sensitivities is continuously evolving. Whether you’re a practitioner or managing your own sensitivities, committing to ongoing education through reputable sources is indispensable. Knowledge empowers informed health decisions, fostering a foundation for wellness and vitality.
- Champion Personalized Care: The individuality of food sensitivities necessitates tailored care strategies. We encourage practitioners to build informed, collaborative relationships with their clients and urge individuals to seek practitioners who recognize the intricacies of food sensitivities. Together, you can forge a path to improved health and well-being.
Navigating the complexities of food sensitivities poses challenges, yet armed with the correct knowledge, tools, and support, managing these sensitivities effectively to enhance your quality of life is within reach. Whether you're on a personal health journey or guiding others, remember: informed, personalized care is paramount.
Join us in our mission to elevate health and wellness through informed, personalized care by exploring our health coaching certification programs. Together, we can make a meaningful impact on the lives of those navigating food sensitivities. Schedule a call today to speak with an Admissions Counselor to begin your journey to understanding the world of food sensitivities.